A HIPAA compliant cloud backup isn't just a place to stash copies of your files. It's a specialized service designed from the ground up to meet the strict security and privacy rules of the Health Insurance Portability and Accountability Act. This means it must have end-to-end encryption, ironclad access controls, and a signed Business Associate Agreement (BAA), which is the legal glue ensuring your data's protection. For any practice handling patient data, this is foundational.
Why HIPAA Compliant Cloud Backup Is Essential

Whether you’re a solo dental practice or a growing law firm, protecting client and patient data is more than just good business—it's the law. As we've all moved to electronic records, that data is easier to use but also much easier to lose.
A simple hard drive crash, an accidental "delete," or a targeted cyberattack can wipe you out. We’re talking about catastrophic data loss, bringing your operations to a grinding halt and opening you up to severe regulatory penalties. This is exactly why a HIPAA compliant cloud backup strategy isn’t just a nice-to-have; it's completely non-negotiable.
More Than Just Storage
It's a common mistake to think any old cloud storage service will do the trick. They are worlds apart.
Think of a standard cloud service like a personal lockbox. You've got the key, and it offers some basic protection. A HIPAA compliant solution, on the other hand, is like a guarded bank vault. It’s not just about locking the data away. It’s a complete security system that includes:
- End-to-End Encryption: Your data gets scrambled into unreadable code before it even leaves your office, stays scrambled while traveling online, and remains that way while stored in the data center.
- Strict Access Controls: Only people you specifically authorize can get to the data, and every single action they take is logged.
- Audited Disaster Recovery: The provider has tested, proven plans to get your data back to you quickly and securely when disaster strikes.
A huge misconception is that using a big-name cloud provider automatically makes you compliant. The truth is that compliance is a shared responsibility. The provider gives you the secure vault, but your organization is responsible for using the locks correctly.
The High Stakes of Non-Compliance
Failing to have a proper backup and disaster recovery plan is one of the most frequent HIPAA violations we see. The consequences can be devastating and go way beyond a simple fine.
A data breach can trigger massive financial penalties from the Office for Civil Rights (OCR), not to mention the cost of lawsuits and the permanent damage to your reputation. Patients and clients trust you with their most private information. Losing that trust can cripple a practice overnight.
On top of that, cyberattacks are a constant threat. Ransomware loves to target healthcare providers because they know how critical that data is. Without a secure, separate backup, you might be forced to pay a huge ransom with zero guarantee you'll ever see your files again. Understanding how to prevent ransomware attacks is your first line of defense, but a compliant backup is your ultimate safety net. It ensures that even if your main systems are locked down, you have a clean copy ready to restore.
Decoding the HIPAA Security Rule for Data Backups

The HIPAA Security Rule isn't a friendly suggestion; it's a federal mandate that spells out exactly how electronic protected health information (ePHI) must be secured. When you're putting together a HIPAA compliant cloud backup strategy, this rule is your non-negotiable blueprint. It goes way beyond just storing files—it demands a structured, layered defense for your data.
Think of the Security Rule as a three-legged stool holding up your entire compliance effort. If one leg is wobbly, the whole thing comes crashing down. Those three legs are the Administrative, Physical, and Technical Safeguards, each with its own unique job in protecting patient data in your backups.
The Administrative Safeguards Playbook
First up are the Administrative Safeguards. These are the human side of security—your organization's official playbook. This isn't about fancy software, but about the policies, procedures, and people responsible for protecting ePHI. This is where you write down the game plan.
Your "playbook" needs to cover a few critical bases:
- Security Management Process: This is the heart of it all. You have to perform a formal risk analysis to spot potential threats to your ePHI and then put security measures in place to knock them down.
- Assigned Security Responsibility: You can't just hope someone handles it. You must name a specific person (like a Security Officer) who is officially in charge of creating and enforcing your security policies.
- Workforce Security: This means having clear procedures for who gets to see ePHI, how they're supervised, and what happens when an employee leaves. It’s all about managing access.
- Contingency Plan: Having a documented plan that includes data backup, disaster recovery, and how to operate in an emergency isn't optional—it's a specific requirement.
Basically, Administrative Safeguards make sure your team knows the rules and has a clear plan for both protecting data and responding if something goes wrong.
Physical Safeguards: The Locks and Keys
Next, we have the Physical Safeguards. These are the actual locks, keys, and security cameras protecting the hardware where your data is stored. Just because you're using a cloud backup provider doesn't let you off the hook here. It just shifts the responsibility to making sure your provider has rock-solid physical security.
The Security Rule is technology-neutral, meaning it doesn't prescribe specific software or hardware. Instead, it sets the standard for what must be achieved, leaving the 'how' up to the organization and its business associates.
Your chosen HIPAA compliant cloud backup provider must be able to prove they have tight physical controls at their data centers. This means things like controlled access to the facility, secure workstations, and strict policies for any physical media. It’s the digital version of locking the server room door and only giving keys to authorized staff. This is precisely why you need to check a provider's data center certifications, like SOC 2.
Technical Safeguards: The Digital Alarms
Finally, we have the Technical Safeguards. These are the digital protections built right into the technology itself. Think of them as the firewalls, encryption, and audit logs that act as the alarms and armored walls for your ePHI.
Some of the key requirements here include:
- Access Control: You need to implement tech policies that only allow authorized people to access ePHI. This usually means unique user IDs, automatic logoffs, and, of course, encryption.
- Audit Controls: Your systems must be able to log and let you examine activity. Who accessed what file, and when? You need to have those records.
- Integrity Controls: You must have measures in place to make sure ePHI isn't accidentally or maliciously changed or deleted.
- Transmission Security: This is absolutely critical for cloud backups. You have to protect ePHI while it's in transit over a network. This is why end-to-end encryption is a deal-breaker feature.
When you put these three safeguards together, you create a powerful "defense-in-depth" strategy. Your data is protected by policies (administrative), physical security, and technology. A weak link in any one of these areas can easily lead to a breach and a world of compliance headaches.
The Critical Role of a Business Associate Agreement
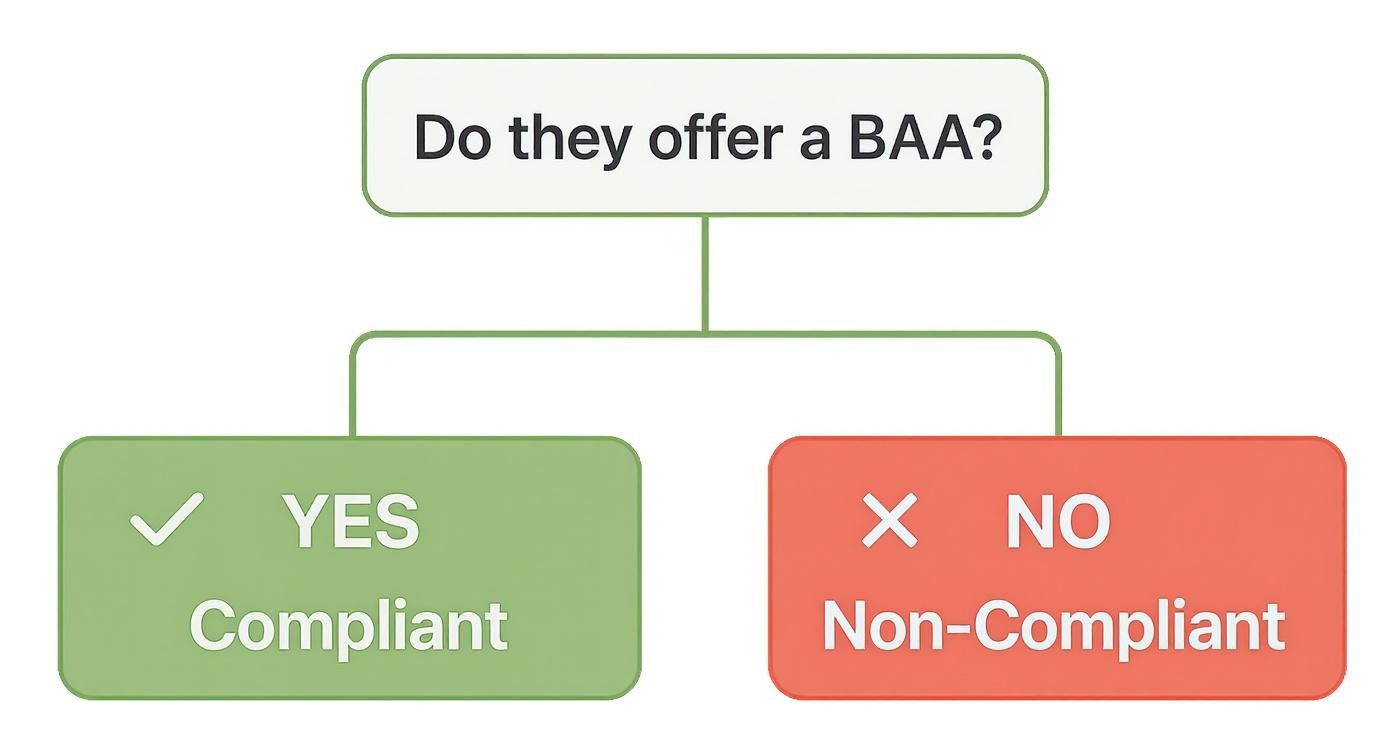
When you bring a cloud backup service into the fold, especially one that will be handling your patients' sensitive data, your relationship is built on more than just a handshake. It's built on a formal, legal contract called a Business Associate Agreement (BAA). This is the absolute bedrock of your partnership and the single most important document legally binding your provider to protect that information.
It’s easy to fall into the trap of thinking that any big-name cloud provider is automatically safe for healthcare use. That’s a massive—and dangerous—misunderstanding. Without a signed BAA, you have zero legal assurance that the provider will safeguard electronic protected health information (ePHI) according to HIPAA’s strict rules. The BAA is what officially hands them the responsibility, making them just as accountable as you are.
Think of it this way: hiring a cloud provider without a BAA is like giving a security firm the keys to your office but never signing a contract. You’ve let them in, but there’s no written agreement spelling out their duties, what happens if something goes wrong, or who’s liable if there’s a break-in. The BAA is that essential contract, turning a simple vendor into a legally compliant partner.
What a Compliant BAA Must Contain
A proper BAA isn't some one-page formality you sign and file away. It's a detailed agreement that lays out exactly what your cloud backup provider (the "Business Associate") can and can't do with your data. For it to be valid under HIPAA, it needs to cover some very specific ground.
At its core, the BAA must clearly define how the provider is allowed to use ePHI and state that they won't use or share it in any way that would violate the HIPAA Privacy Rule.
A truly compliant agreement will always include these key components:
- Specific Security Duties: The BAA must legally require the provider to implement all necessary safeguards—Administrative, Physical, and Technical—to protect the ePHI they're storing for you.
- Breach Notification Procedures: The contract must spell out exactly how and when the provider will report any security incidents or data breaches. This includes firm timelines and the type of information they are required to give you.
- Rules for Subcontractors: If your provider uses other companies to help them (subcontractors), the BAA must ensure those third parties are also bound by the same tough HIPAA rules.
- Data Return or Destruction: It needs to state what happens when your contract ends. The provider must either return all your ePHI or securely destroy it.
This level of detail leaves no room for confusion about who is responsible for what.
The BAA and the Shared Responsibility Model
Once that BAA is signed, you've officially entered into a "shared responsibility model." While your provider takes on the legal duty to protect their infrastructure and the data they store, your organization still holds responsibility for how you use that service.
A signed BAA is not a "get out of jail free" card. It defines your provider's responsibilities, but your practice is still responsible for correctly configuring access controls, managing user permissions, and ensuring your own internal security practices are sound.
For example, your cloud provider is responsible for making sure their data centers are physically secure and that your data is encrypted. But it's still your job to make sure only authorized employees have the passwords to access those backups.
This is precisely why a BAA is so crucial. It draws a clear line in the sand, defining where the provider's duties end and yours begin. Without this legally binding document, that line gets blurred. And if a breach happens, all the liability could fall squarely on your shoulders, leading to crippling fines and a damaged reputation you might never recover from.
How to Choose the Right Cloud Backup Provider
Picking a cloud backup provider is easily one of the most critical security decisions you'll make for your practice. You're not just finding a digital locker for your files; you're handing over the keys to your most sensitive data and trusting a partner to keep you on the right side of the law.
The market is flooded with companies all claiming to have the perfect solution. But a genuinely HIPAA compliant cloud backup service requires you to look past the marketing promises.
You have to cut through the noise by asking tough questions and demanding clear, documented proof. This isn't about ticking boxes on a feature list. It's about digging into the provider's security culture, their infrastructure, and the legal promises they're willing to make. Let’s walk through a practical roadmap to help you find a partner that actually fits your security needs.
HIPAA Eligible vs. HIPAA Compliant
First things first, you need to grasp the massive difference between a provider being "HIPAA eligible" and one offering a truly "HIPAA compliant" solution. This isn't just wordplay—it's about where the responsibility for security ultimately lands.
A HIPAA-eligible platform gives you the secure building blocks—the infrastructure and tools—but leaves the entire assembly process up to you. You’re on the hook for everything: configuring encryption, setting up access controls, and double-checking that every single setting is locked down according to HIPAA rules. It's a high-stakes DIY project that can easily go wrong if you don’t have a dedicated security expert on your team.
On the other hand, a HIPAA-compliant solution, which is usually a fully managed service, takes that heavy lifting off your plate. They deliver an environment that’s already configured to meet HIPAA’s strict requirements. This drastically cuts down on your workload and, more importantly, the risk of a simple human error causing a major compliance breach. For most small and mid-sized practices, a managed solution is by far the smarter, safer bet.
Your Essential Provider Vetting Checklist
When you're talking to potential providers, be direct and specific. If their answers are vague, consider it a giant red flag. Use this checklist to guide your conversations and make sure you cover all the non-negotiables.
- Business Associate Agreement (BAA): This is the absolute deal-breaker. Will they sign a BAA before you transfer a single byte of ePHI? If not, the conversation is over.
- Encryption Methods: Get specific about how they encrypt data. You need confirmation that they use strong, modern encryption (like AES-256) for your data both at-rest (while it's stored on their servers) and in-transit (as it travels across the internet).
- Data Center Security: What's going on at their physical locations? Ask to see third-party audit reports and certifications like SOC 2 Type II, which proves their security controls have been tested over time.
- Disaster Recovery Capabilities: Do they have a documented plan for when things go wrong? You need to know their Recovery Time Objectives (RTOs) and Recovery Point Objectives (RPOs) to be sure they can get you back online in a timeframe your practice can handle.
- Access Controls and Audit Trails: Who can see your data, and how do they prove it? The service must allow you to set role-based access controls and provide detailed audit logs that track every touch, view, and change made to your backed-up files.
The takeaway here is simple: if a provider won't sign a BAA, they're not an option for your ePHI. End of story.
Of course, the major cloud players have stepped up to offer solutions for healthcare data. Big names like Amazon Web Services (AWS), Microsoft Azure, and Google Cloud all provide services that can be made HIPAA compliant. The catch is that their models differ significantly.
Here's a quick comparison to illustrate the different approaches you'll encounter.
Cloud Provider HIPAA Compliance Model Comparison
| Provider/Type | Compliance Model | Key Feature | Best For |
|---|---|---|---|
| AWS, Azure, Google Cloud | Infrastructure (IaaS) | Provides HIPAA-eligible "building blocks" | Organizations with deep in-house IT security expertise |
| Fully Managed Service | Compliance-as-a-Service | Pre-configured, compliant environment | Small to mid-sized businesses without a dedicated security team |
| Hybrid Model | Managed on top of IaaS | Combines IaaS flexibility with expert management | Businesses needing custom setups with guided compliance |
While AWS might offer a toolkit for building a secure architecture, you are still the one who has to build it correctly. Azure provides HIPAA-ready templates, but they still need proper deployment and management. As a great resource from HIPAA Vault on HIPAA compliant cloud storage explains, the responsibility often falls back on the customer.
Ultimately, choosing the right partner comes down to finding a provider whose security posture you can trust without reservation. Taking the time to do this homework is the only way to protect your patients, your practice, and your own peace of mind.
For many practices, the simplest and most effective route is to work with an expert in managed IT services for businesses. A good partner can handle this entire process, ensuring your backups are not just compliant, but perfectly suited to how your business actually runs.
Common Mistakes in HIPAA Cloud Backup Implementation
Setting up a HIPAA compliant cloud backup solution feels like walking a tightrope. One small misstep can create a massive compliance gap, and unfortunately, even well-intentioned dental practices and law firms often stumble into the same common pitfalls. These aren't just technical glitches; they're fundamental misunderstandings that can leave patient data wide open to risk.
One of the most common—and costly—mistakes is getting the timing wrong with the Business Associate Agreement (BAA). In a rush to get protected, some businesses start uploading ePHI to a cloud service before the BAA is actually signed. That single move puts them immediately out of compliance. Think of the BAA as the legal foundation of your partnership, not a piece of paperwork you can backdate. Without it, your cloud provider has zero legal obligation under HIPAA to protect your data, and you're the one left holding the bag if a breach happens.
Another huge misstep is buying into the myth that cloud storage is automatically secure. This comes from a fuzzy understanding of the shared responsibility model. Yes, the cloud provider secures the big stuff—the physical data centers and their network. But you are responsible for configuring the service correctly and securely. Just moving your files to a "HIPAA eligible" cloud doesn't magically make you compliant.
Misconfiguring Access and Neglecting Tests
Beyond the initial setup, a couple of ongoing mistakes can make an otherwise solid backup plan totally worthless when you actually need it. The first is sloppy access control. This usually looks like using generic or shared logins for everyone or giving employees way more permissions than they need to do their jobs.
Good access control is all about the principle of least privilege. It’s simple: each user should only have access to the bare minimum of data required for their role. When you get this wrong, you're creating an easy-access lane for both internal slip-ups and external attacks. For instance, if your receptionist's login has full admin rights to the backup system, a single successful phishing email could lead to every single patient record being stolen or deleted.
The second, and maybe most dangerous, mistake is the "set it and forget it" mindset. So many businesses do the hard work of setting up backups but then fail to regularly test the data restoration process. They see the "backup successful" notification and assume everything is fine.
Picture this: a dental clinic gets hit with ransomware. The office manager confidently goes to restore from the backup, only to find the files are corrupted or the restore process fails. That's a nightmare scenario, and it happens all the time. It turns a manageable problem into a potential business-ending disaster. Regular, documented testing is the only way to know for sure that your safety net will actually catch you.
Underestimating the Current Threat Landscape
Ignoring the sheer intensity of modern cyber threats is a mistake that makes every other one worse. The stakes have never been higher. In the first half of a recent year alone, reported healthcare data breaches shot up 23% compared to the year before, with ransomware leading the charge. With the average price tag of a healthcare data breach now hitting around $11 million per incident, even a small practice is a juicy target. You can see more of the scary numbers in these healthcare breach statistics on ReadyCloud.com. This brutal reality makes having a flawless HIPAA compliant cloud backup and recovery plan absolutely non-negotiable.
Your Action Plan for Compliant Data Backups

Alright, let's turn all that theory into a practical, secure backup strategy. It can feel like a mountain to climb, but if you break it down into a clear roadmap, you can build a compliant and genuinely effective plan without missing a single critical step. This is your action plan for getting it done right.
The first step, always, is to run a thorough risk assessment. It’s simple: you can't protect what you don't understand. This means digging in and identifying every single place where electronic protected health information (ePHI) is created, stored, or sent. From there, you can start pinpointing the real-world threats to that data.
Once you have a clear picture of your risks, you can figure out your backup scope and schedule. Let’s be honest, not all data is created equal. You need to decide which systems are absolutely essential for your day-to-day operations and need more frequent backups. This helps you establish your Recovery Point Objective (RPO)—in other words, how much data you can stomach losing in a worst-case scenario.
Vetting Providers and Executing a BAA
With your own requirements clearly defined, you can start looking at potential providers for your HIPAA compliant cloud backup. Create a checklist to evaluate their encryption methods, data center certifications, and how they handle disaster recovery.
Most importantly, any provider you consider must be willing to sign a Business Associate Agreement (BAA) before you hand over a single byte of data.
A BAA is the non-negotiable legal contract that makes your provider a partner in compliance. Signing it after the fact is a direct violation and exposes your practice to significant risk.
After you've picked a partner and have that signed BAA in hand, it's time to get everything set up. This is more than just installing some software. You have to correctly configure who can access the data, set up your encryption keys, and establish automated backup schedules that match the policies you just created.
Testing Your Data Recovery Plan
This last step is the one people often skip, but it’s the most crucial of all: regularly test your data recovery plan. A backup is completely useless if you can't actually restore from it. You need to perform test restores of different files, folders, and even entire systems to make sure everything is working and that your team knows exactly what to do when disaster strikes.
This process does two things. It confirms your backups are viable and helps you nail down your Recovery Time Objective (RTO)—how quickly you can get back up and running after an outage.
If the thought of restoring data on your own is stressful, a professional data recovery service can provide expert guidance and support. Consistent testing is the only way to be absolutely sure your safety net will actually catch you when you need it most.
Got Questions About HIPAA Backups? We've Got Answers.
When it comes to HIPAA compliant cloud backups, it’s easy to get tangled up in the details. It's a common point of confusion, and we hear a lot of the same questions from practices trying to get it right. Let's clear up a few of the most common ones.
Can We Just Use Google Drive or Dropbox for Our Backups?
This is a big one. The short answer is no—at least, not the standard, free versions you use for personal files. Those consumer accounts are not HIPAA compliant right out of the box.
However, the upgraded business versions of these services, like Google Workspace or Dropbox Business, can be part of a compliant plan. The catch? You must have a signed Business Associate Agreement (BAA) with them, and you're the one responsible for configuring all the security settings correctly. It puts the entire burden of setup and maintenance squarely on your shoulders.
How Often Do We Really Need to Test Our Disaster Recovery Plan?
HIPAA is famously vague here, not giving a hard and fast deadline. But if you ask anyone in the IT world, the consensus is clear: test your data recovery plan at least annually.
And if you make any major changes to your IT setup—like getting a new server or switching practice management software—you should test it more often. A backup you haven't tested is just a hope, not a plan. Regular testing is the only way to know for sure that you can get back up and running after a disaster.
What's the Real Difference Between a "Backup" and an "Archive"?
It’s easy to mix these up, but they serve two totally different purposes.
A backup is your emergency parachute. It's a recent copy of your active data, designed to get you back in business quickly after a server crash, ransomware attack, or even just an accidental deletion. Think of it as your "get out of jail free" card for data loss.
An archive, on the other hand, is more like a long-term storage unit. It’s for old data you don't use every day but have to keep for legal or compliance reasons. Archives are secure, but they aren't built for speed. Restoring from an archive can be a much slower process.
Key Takeaway: No matter which service you use, your strategy is only compliant if it's built on two pillars: a signed Business Associate Agreement (BAA) with your provider and a written contingency plan that you actually test. If you're missing either one, you're not meeting HIPAA's requirements.
Keep your business running without IT headaches.
GT Computing provides fast, reliable support for both residential and business clients. Whether you need network setup, data recovery, or managed IT services, we help you stay secure and productive.
Contact us today for a free consultation.
Call 203-804-3053 or email Dave@gtcomputing.com
.